Definition
Skin grafting is a surgical procedure in which skin or a skin substitute is placed over a burn or non-healing wound.Purpose
A skin graft is used to permanently replace damaged or missing skin or to provide a temporary wound covering. This covering is necessary because the skin protects the body from fluid loss, aids in temperature regulation, and helps prevent disease-causing bacteria or viruses from entering the body. Skin that is damaged extensively by burns or non-healing wounds can compromise the health and well-being of the patient.Demographics
Although anyone can be involved in a fire and need a skin graft, the population groups with a higher risk of fire-related injuries and deaths include:- children four years old and younger
- adults 65 years and older
- African Americans and Native Americans
- low-income Americans
- persons living in rural areas
- persons living in manufactured homes (trailers) or substandard housing
Description
The skin is the largest organ of the human body. It is also known as the integument or integumentary system because it covers the entire outside of the body. The skin consists of two main layers: the outer layer, or epidermis, which lies on and is nourished by the thicker dermis. These two layers are approximately 0.04–0.08 in (1–2 mm) thick. The epidermis consists of an outer layer of dead cells called keratinocytes, which provide a tough protective coating, and several layers of rapidly dividing cells just beneath the keratinocytes. The dermis contains the blood vessels, nerves, sweat glands, hair follicles, and oil glands. The dermis consists mainly of connective tissue, which is largely made up of a protein called collagen. Collagen gives the skin its flexibility and provides structural support. The fibroblasts that make collagen are the main type of cell in the dermis.Skin varies in thickness in different parts of the body; it is thickest on the palms and soles of the feet, and thinnest on the eyelids. In general, men have thicker skin than women, and adults have thicker skin than children. After age 50, however, the skin begins to grow thinner again as it loses its elastic fibers and some of its fluid content.
Injuries treated with skin grafts
Skin grafting is sometimes done as part of elective plastic surgery procedures, but its most extensive use is in the treatment of burns. For first or second-degree burns, skin grafting is generally not required, as these burns usually heal with little or no scarring. With third-degree burns, however, the skin is destroyed to its full depth, in addition to damage done to underlying tissues. People who suffer third-degree burns often require skin grafting.Wounds such as third-degree burns must be covered as quickly as possible to prevent infection or loss of fluid. Wounds that are left to heal on their own can contract, often resulting in serious scarring; if the wound is large enough, the scar can actually prevent movement of limbs. Non-healing wounds, such as diabetic ulcers, venous ulcers, or pressure sores, can be treated with skin grafts to prevent infection and further progression of the wounded area.
Types of skin grafts
The term "graft" by itself commonly refers to either an allograft or an autograft. An autograft is a type of graft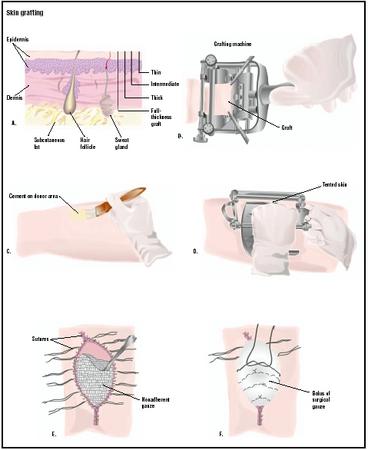
Skin grafts may be used in several thicknesses (A). To begin the procedure, a special cement is used on the donor skin area (C). The grafting machine is applied to the area, and a sample taken (D). After the graft is stitched to the recipient area, it is covered with nonadherent gauze (E) and a layer of fluffy surgical gauze held in place with suture (F). (
Illustration by GGS Inc.
) SPLIT-THICKNESS GRAFTS. The most important part of any skin graft procedure is proper preparation of the wound. Skin grafts will not survive on tissue with a limited blood supply (cartilage or tendons) or tissue that has been damaged by radiation treatment. The patient's wound must be free of any dead tissue, foreign matter, or bacterial contamination. After the patient has been anesthetized, the surgeon prepares the wound by rinsing it with saline solution or a diluted antiseptic (Betadine) and removes any dead tissue by débridement. In addition, the surgeon stops the flow of blood into the wound by applying pressure, tying off blood vessels, or administering a medication (epinephrine) that causes the blood vessels to constrict.
Following preparation of the wound, the surgeon then harvests the tissue for grafting. A split-thickness skin graft involves the epidermis and a little of the underlying dermis; the donor site usually heals within several days. The surgeon first marks the outline of the wound on the skin of the donor site, enlarging it by 3–5% to allow for tissue shrinkage. The surgeon uses a dermatome (a special instrument for cutting thin slices of tissue) to remove a split-thickness graft from the donor site. The wound must not be too deep if a split-thickness graft is going to be successful, since the blood vessels that will nourish the grafted tissue must come from the dermis of the wound itself. The graft is usually taken from an area that is ordinarily hidden by clothes, such as the buttock or inner thigh, and spread on the bare area to be covered. Gentle pressure from a well-padded dressing is then applied, or a few small sutures used to hold the graft in place. A sterile nonadherent dressing is then applied to the raw donor area for approximately three to five days to protect it from infection.
FULL-THICKNESS GRAFTS. Full-thickness skin grafts may be necessary for more severe burn injuries. These grafts involve both layers of the skin. Full-thickness autografts are more complicated than partial-thickness grafts, but provide better contour, more natural color, and less contraction at the grafted site. A flap of skin with underlying muscle and blood supply is transplanted to the area to be grafted. This procedure is used when tissue loss is extensive, such as after open fractures of the lower leg, with significant skin loss and underlying infection. The back and the abdomen are common donor sites for full-thickness grafts. The main disadvantage of full-thickness skin grafts is that the wound at the donor site is larger and requires more careful management. Often, a split-thickness graft must be used to cover the donor site.
A composite skin graft is sometimes used, which consists of combinations of skin and fat, skin and cartilage, or dermis and fat. Composite grafts are used in patients whose injuries require three-dimensional reconstruction. For example, a wedge of ear containing skin and cartilage can be used to repair the nose.
A full-thickness graft is removed from the donor site with a scalpel rather than a dermatome. After the surgeon has cut around the edges of the pattern used to determine the size of the graft, he or she lifts the skin with a special hook and trims off any fatty tissue. The graft is then placed on the wound and secured in place with absorbable sutures.
Aftercare
Once a skin graft has been put in place, it must be maintained carefully even after it has healed. Patients who have grafts on their legs should remain in bed for seven to 10 days with their legs elevated. For several months, the patient should support the graft with an Ace bandage or Jobst stocking. Grafts on other areas of the body should be similarly supported after healing to decrease the amount of contracture.Grafted skin does not contain sweat or oil glands, and should be lubricated daily for two to three months with mineral oil or another bland oil to prevent drying and cracking.
Aftercare of patients with severe burns typically includes psychological or psychiatric counseling as well as wound care and physical rehabilitation, particularly if the patient's face has been disfigured. The severe pain and lengthy period of recovery involved in burn treatment are often accompanied by anxiety and depression. If the patient's burns occurred in combat, a transportation disaster, terrorist attack, or other fire involving large numbers of people, he or she is at high risk of developing post-traumatic stress disorder (PTSD). Doctors treating the survivors of a nightclub fire in Rhode Island in February 2003 gave them anti-anxiety medications within a few days of the tragedy in order to reduce the risk of PTSD.
Risks
The risks of skin grafting include those inherent in any surgical procedure that involves anesthesia. These include reactions to the medications, breathing problems, bleeding, and infection. In addition, the risks of an allograft procedure include transmission of an infectious disease from the donor.The tissue for grafting and the recipient site must be as sterile as possible to prevent later infection that could result in failure of the graft. Failure of a graft can result from inadequate preparation of the wound, poor blood flow to the injured area, swelling, or infection. The most common reason for graft failure is the formation of a hematoma, or collection of blood in the injured tissues.
Normal results
A skin graft should provide significant improvement in the quality of the wound site, and may prevent the serious complications associated with burns or non-healing wounds. Normally, new blood vessels begin growing from the donor area into the transplanted skin within 36 hours. Occasionally, skin grafts are unsuccessful or don't heal well. In these cases, repeat grafting is necessary. Even though the skin graft must be protected from trauma or significant stretching for two to three weeks following split-thickness skin grafting, recovery from surgery is usually rapid. A dressing may be necessary for one to two weeks, depending on the location of the graft. Any exercise or activity that stretches the graft or puts it at risk for trauma should be avoided for three to four weeks. A one to two-week hospital stay is most often required in cases of full-thickness grafts, as the recovery period is longer.Morbidity and mortality rates
According to the American Burn Association, there are more than 1 million burn injuries in the United States each year that require medical attention. Approximately one-half of these require hospitalization, and roughly 25,000 of those burn patients are admitted to a specialized burn unit. About 4,500 people die from burns each year in the United States.In the United States, someone dies in a fire nearly every two hours, on average, and another person is injured every 23 minutes. Approximately half the deaths occur in homes without smoke alarms. In addition to deaths resulting directly from burns, as many as 10,000 Americans die every year of burn-related infections, pneumonia being the most common infectious complication among hospitalized burn patients.
The average size of a burn injury in a patient admitted to a burn center is approximately 14% of the total body surface area. Smaller burns covering 10% of the total body area or less account for 54% of burn center admissions, while larger burns covering 60% or more account for 4% of admissions. About 6% of patients admitted to burn centers do not survive, mostly as a result of having suffered severe inhalation injuries in a fire.
Treatment for severe burns has improved dramatically in the past 20 years. Today, patients can survive with burns covering up to about 90% of the body, although they often face permanent physical impairment.
Alternatives
There has been great progress in the development of artificial skin replacement products in recent years. Although nothing works as well as the patient's own skin, artificial skin products are important due to the limitation of available skin for allografting in severely burned patients. Unlike allographs and xenographs, artificial skin replacements are not rejected by the patient's body and actually encourage the generation of new tissue. Artificial skin usually consists of a synthetic epidermis and a collagen-based dermis. The artificial dermis consists of fibers arranged in a lattice that act as a template for the formation of new tissue. Fibroblasts, blood vessels, nerve fibers, and lymph vessels from surrounding healthy tissue grow into the collagen lattice, which eventually dissolves as these cells and structures build a new dermis. The synthetic epidermis, which acts as a temporary barrier during this process, is eventually replaced with a split-thickness autograft or with an epidermis cultured in the laboratory from the patient's own epithelial cells.Several artificial skin products are available for burns or non-healing wounds, including Integra®, Dermal Regeneration Template® (from Integra Life Sciences Technology), Apligraft® (Novartis), Transcyte® (Advance Tissue Science), and Dermagraft®. Researchers have also obtained promising results growing or cultivating the patient's own skin cells in the laboratory. These cultured skin substitutes reduce the need for autografts and can reduce the complications of burn injuries. Laboratory cultivation of skin cells may improve the prognosis for severely burned patients with third-degree burns over 50% of their body. The recovery of these patients has been hindered by the limited availability of uninjured skin from their own bodies for grafting. Skin substitutes may also reduce treatment costs and the length of hospital stays. In addition, other research has demonstrated the possibility of using stem cells collected from bone marrow or blood for use in growing skin grafts.
Patients with less severe burns are usually treated in a doctor's office or a hospital emergency room. Patients with any of the following conditions, however, are usually transferred to hospitals with specialized burn units: third-degree burns; partial-thickness burns over 10% of their total body area; electrical or chemical burns; smoke inhalation injuries; or preexisting medical disorders that could complicate management, prolong recovery, or affect mortality. In addition, burned children in hospitals without qualified personnel should be admitted to a hospital with a burn unit. A surgical team that specializes in burn treatment and skin grafts will perform the necessary procedures. The team may include neurosurgeons, ophthalmologists, oral surgeons, thoracic surgeons, psychiatrists, and trauma specialists as well as plastic surgeons and dermatologists.
POSTED BY ATTORNEY RENE G. GARCIA
Some of our clients have suffered these kinds of injuries due to a serious accident or malpractice. The Garcia Law Firm, P.C. was able to successfully handle these types of cases. For a free consultation please call us at 1-866- SCAFFOLD or 212-725-1313.
No comments:
Post a Comment