Definition
Tendon repair refers to the surgical repair of damaged or torn tendons, which are cord-like structures made of strong fibrous connective tissue that connect muscles to bones. The shoulder, elbow, knee, and ankle joints are the most commonly affected by tendon injuries.Purpose
The goal of tendon repair is to restore the normal function of joints or their surrounding tissues following a tendon laceration.Demographics
Tendon injuries are widespread in the general adult population. They are more common among people whose occupations or recreational athletic activities require repetitive motion of the shoulder, knee, elbow, or ankle joints. Injuries to the tendons in the shoulder often occur among baseball players, window washers, violinists, dancers, carpenters, and some assembly line workers. Rowers are at increased risk for injuries to the forearm tendons. The repetitive stresses of classical ballet, running, and jogging may damage the Achilles tendon at the back of the heel. So-called tennis elbow, which occurs in many construction workers, highway crews, maintenance workers, and baggage handlers as well as professional golfers and tennis players, is thought to affect 5% of American adults over the age of 30.Women in all age brackets are at greater risk than men for injuries to the tendons in the elbow and knee joints. It is thought that injuries in these areas are related to the slightly greater looseness of women's joints compared to those in men.
Description
Local, regional or general anesthesia is administered to the patient depending on the extent and location of tendon damage. With a general anesthetic, the patient is asleep during surgery. With a regional anesthetic, a specific region of nerves is anesthetized; with a local anesthetic, the patient remains alert during the surgery, and only the incision location is anesthetized.After the overlying skin has been cleansed with an antiseptic solution and covered with a sterile drape, the surgeon makes an incision over the injured tendon. When the tendon has been located and identified, the surgeon sutures the damaged or torn ends of the tendon together. If the tendon has been severely injured, a tendon graft may be required. This is a procedure in which a piece of tendon is taken from the foot or other part of the body and used to repair the damaged tendon. If required, tendons are reattached to the surrounding connective tissue. The surgeon inspects the area for injuries to nerves and blood vessels, and closes the incision.
Diagnosis/Preparation
Diagnosis of a tendon injury is usually made when the patient consults a doctor about pain in the injured area. The doctor will usually order radiographs and other imaging studies of the affected joint as well as taking a history and performing an external physical examination in the office. In some cases fluid will be aspirated (withdrawn through a needle) from the joint to check for signs of infection, bleeding, or arthritis.Prior to surgery, the patient is asked not to eat or drink anything, even water. A few days before the operation, patients are also instructed to stop taking such over-thecounter pain medications as aspirin or ibuprofen. If the patient has a splint or cast, it is removed before surgery.
To prepare for surgery, the patient typically reports to a preoperative nursing unit, where he or she changes into a hospital gown. Next, the patient is taken to a preoperative holding area, where an anesthesiologist administers an intravenous sedative. The patient is then taken to the operating room .
Aftercare
Patients are asked to have someone drive them home after tendon repair surgery. Healing may take as long as 6 weeks, during which the injured part may be immobilized in a splint or cast. Patients are asked not to use the injured tendon until the physician gives permission. The physician will decide how long to rest the tendon. It should not be used for lifting heavy objects or walking. Patients are also asked to avoid driving until the physician gives the go-ahead. To reduce swelling and pain, they should keep the injured limb lifted above the level of the heart as much as possible for the first few days after surgery.Splints or bandages should be left in place until the next checkup. Patients are advised to keep bandages clean and dry. If patients have a cast, they are asked not to get it wet, to cover it with plastic while bathing, and to avoid exposing the cast to water. Fiberglass casts that get wet may be dried with a hair dryer. Patients are also instructed not to push or lean on the cast to avoid breaking it. If patients have a splint that is held in place with an Ace bandage, they are instructed to ensure that the bandage is not too tight. They are also asked to ensure that
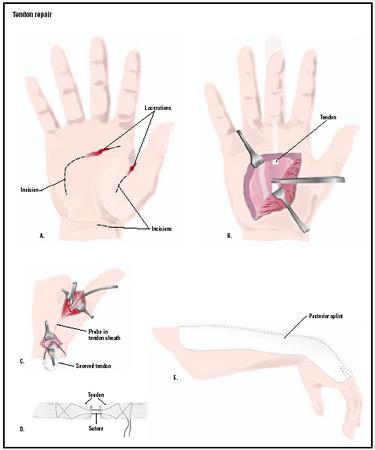
To repair a torn tendon, incisions are made to expose the area for
repair (A). Some tendons can be reattached through one incision (B),
while others require two to access the severed point and the
remaining tendon (C). A special splint that minimizes stretching the
tendons may be worn after surgery (E).
(
Illustration by GGS Inc.
)
Risks
Tendon repair surgery includes the risks associated with any procedure requiring anesthesia, such as reactions to medications and breathing difficulties. Risks associated with any surgery are also present, such as bleeding and infection. Additional risks specific to tendon repair include: formation of scar tissue that may prevent smooth movements (adequate tendon gliding); nerve damage; and partial loss of function in the involved joint.Normal results
Tendon injuries represent a difficult and frustrating problem. Conservative treatment has little if any chance of restoring optimal range of motion in the injured area. Even after surgical repair, a full range of motion is usually not achieved. Permanent loss of motion, joint contractures, weakness and stiffness may be unavoidable. Scar tissue tends to form between the moving surfaces within joints, resulting in adhesions that hamper motion. The surgical repair may also split apart or loosen. Revision surgery may be required to remove scar tissue, insert tendon grafts or other reconstructive procedures. Thus, successful tendon repair depends on many factors. Recovery of the full range of motion is less likely if there is a nerve injury or a broken bone next to the tendon injury; if a long period of time has elapsed between the injury and surgery; if the patient's tissues tend to form thick scars; and if the damage was caused by a crush injury. The location of the injury is also an important factor in determining how well a patient will recover after surgery.Morbidity and mortality rates
Mortality rates for tendon repairs are very low, partly because some of these procedures can be performed with local or regional anesthesia, and partly because most patients with tendon injuries are young or middle-aged adults in good general health. Morbidity varies according to the specific tendon involved; ruptures of the Achilles tendon or shoulder tendons are more difficult to repair than injuries to smaller tendons elsewhere in the body. In addition, some postoperative complications result from patient noncompliance; in one study, two out of 50 patients in the study sample had new injuries within three weeks after surgery because they did not follow the surgeon's recommendations. In general, tendon repairs performed in the United States are reported as having an infection rate of about 1.9%, with other complications ranging between 5.8% and 9.5%.Alternatives
There are no alternatives to surgery for tendon repair as of 2003; however, research is providing encouraging findings. Although there is no presently approved drug that targets this notoriously slow and often incomplete healing process, a cellular substance recently discovered at the Lawrence Berkeley National Laboratory may lead to a new drug that would improve the speed and durability of healing for injuries to tendons and ligaments. The substance, called Cell Density Signal-1, or CDS-1, by its discoverer, cell biologist Richard Schwarz, acts as part of a chemical switch that turns on procollagen production. Procollagen is a protein manufactured in large amounts by embryonic tendon cells. It is transformed outside the cell into collagen, the basic component of such connective tissues as tendons, ligaments or bones. Amgen Inc. is planning to use genetic engineering to bring CDS-1 into mass production.Prolotherapy represents a less invasive alternative to surgery. It is a form of treatment that stimulates the repair of injured or damaged structures. It involves the injection of dextrose or natural glycerin at the exact site of an injury to stimulate the immune system to repair the area. Thus, prolotherapy causes an inflammatory reaction at the exact site of injuries to such structures as ligaments, tendons, menisci, muscles, growth plates, joint capsules, and cartilage to stimulate these structures to heal. Specifically, prolotherapy causes fibroblasts to multiply rapidly. Fibroblasts are the cells that actually make up ligaments and tendons. The rapid production of new fibroblasts means that strong, fresh collagen tissue is formed, which is what is needed to repair injuries to ligaments or tendons.
POSTED BY ATTORNEY RENE G. GARCIA
Some of our clients have suffered these kinds of injuries due to a serious accident or malpractice. The Garcia Law Firm, P.C. was able to successfully handle these types of cases. For a free consultation please call us at 1-866- SCAFFOLD or 212-725-1313.
Read more: http://www.surgeryencyclopedia.com/St-Wr/Tendon-Repair.html#ixzz2TBOrmyiS
No comments:
Post a Comment